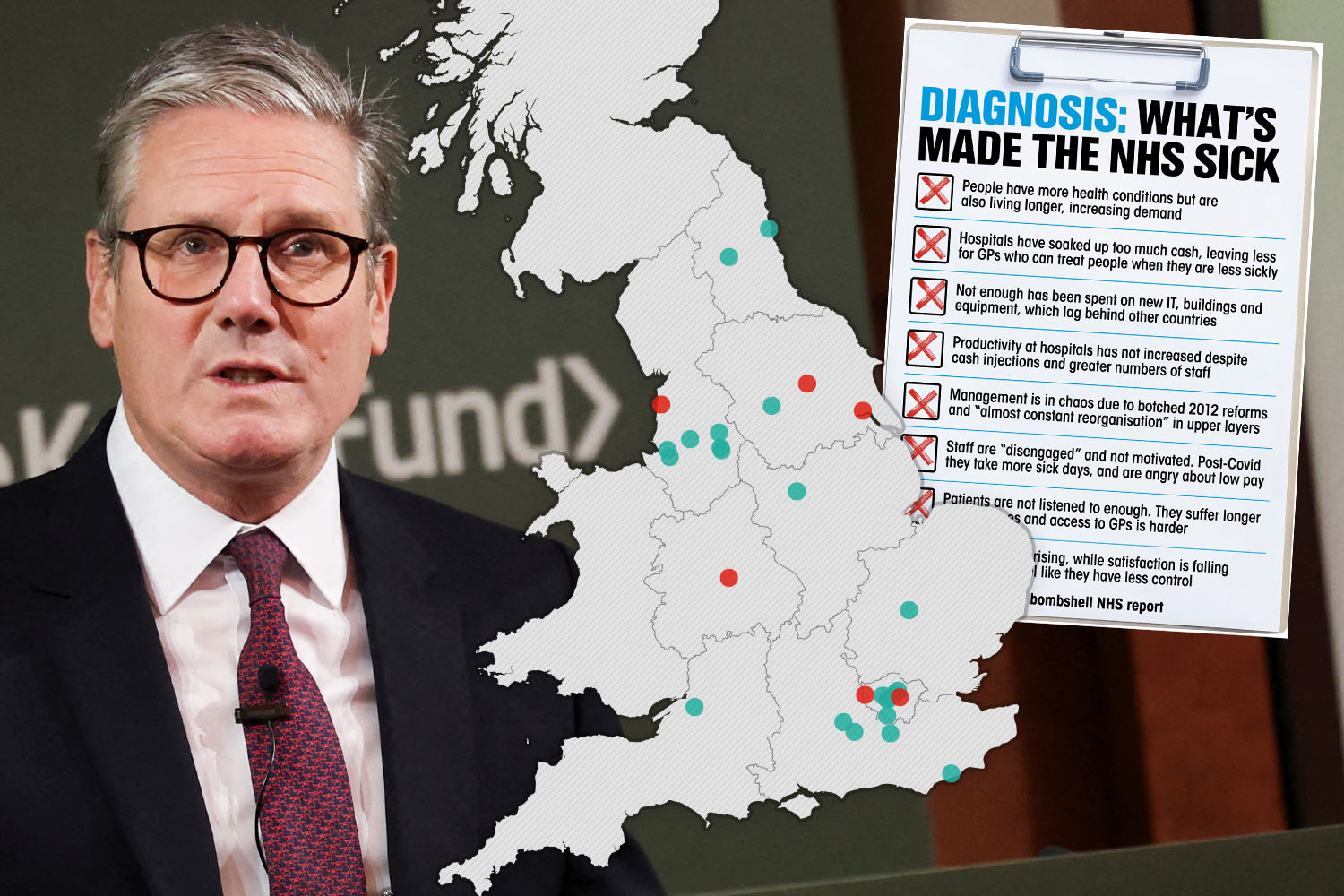
INTERACTIVE maps show the best and worst rated hospitals across England – as Sir Keir Starmer vows to overhaul the “broken” NHS.
As the PM pledged landmark reforms to resuscitate the creaking health service, it was revealed some 49 per cent of hospitals in England were rated ‘Inadequate’ or ‘Requires Improvement’.
3

3
Meanwhile, just under seven per cent of hospitals were deemed to be performing “exceptionally well” and rated ‘Outstanding’.
The remaining 44 per cent of hospitals in England we rated ‘Good’, meaning they’re “performing well and meeting expectations”.
A major report from surgeon Lord Ara Darzi warned the NHS is in critical condition after a decade of “unforgivable” damage.
It said in the best case scenario, the health service will take four years beyond the next election to return to peak performance standards.
In his speech this morning, Sir Keir cited figures of delayed routine treatments of thousands of patients in England, claiming they represent “thousands of avoidable deaths” that “could have been saved”.
And the Labour boss made it his mission to ram through the biggest programme of NHS reform in 75 years – even if it angers stubborn health union leaders.
He warned: “When I arrived as leader of the Labour Party I knew we had to change it. There was a lot of resistance, but we pressed on and did it.
“If there’s one common theme of what I’ve done for a living for some time now it’s coming in and bringing about change. I’m determined we will bring about the change here.”
Postcode lottery
The CQC inspects and regulates health and social care services in England.
It assesses hospitals on five categories, examining whether they’re:
- Safe
- Effective
- Caring
- Responsive
- Well-led
The CQC then produces an overall rating for each hospital, ranging from ‘Outstanding’ to ‘Good’, ‘Requires Improvement’, or ‘Inadequate’.
Medical negligence specialists Patient Claim Line reviewed these numbers to reveal the locations of the best and worst-rated in the country.
A total of 22 hospitals across England were rated ‘Outstanding’, accounting for 6.8 per cent of services.
Meanwhile, 141 hospitals were rated ‘Good’.
But a whopping 152 NHS hospitals in England were deemed to require improvement in their services – meaning they aren’t performing well as they should be.
And a total of six hospitals were deemed to be performing so badly that the CQC thought it necessary to taken enforcement action against the providers – rating the hospitals as ‘Inadequate’.
Found out where in the country these services are and if your nearest hospital is among them.
Worst performing hospitals
Many poorly-rated hospitals were clustered in areas like London, Manchester and Sheffield.
According to Patient Claim Line, the area with the highest number of badly performing hospitals was London, with a total of 16 facilities rated as ‘Requiring Improvement’ or ‘Inadequate’.
Manchester and Sheffield were next, with four poorly rated hospitals each.
Three hospitals in Leicester failed to meet required CQC standards, while Ashford, Hull, Leeds, Liverpool, Newcastle Upon Tyne, Northwood, Orpington, Plymouth, Southampton, Wirral and Worcester had two poorly-rated services each.
CQC inspectors raised concerns about the following worst-rated hospitals:
- The Hillingdon Hospital, Uxbridge
- Hull Royal Infirmary, Hull
- The York Hospital, York
- The Barkantine Centre, London
- Blackpool Victoria Hospital, Blackpool
- Corbett Hospital, Stourbidge
Inspectors at The Hillingdon Hospital raised concerns about a “deterioration in infection prevention and control”, finding “inconsistencies in hand hygiene practice amongst staff”.
Inspectors also noted that there was “poor recognition of sepsis” and they “were not assured that high-risk patient groups were screened for MRSA at pre-admission”.

3
The findings of Lord Darzi’s review on the NHS
LORD Darzi’s report sets out how:
– The health of the nation has deteriorated, with more years spent in ill-health. Factors affecting health, such as poor quality housing, low income and insecure employment, “have moved in the wrong direction over the past 15 years, with the result that the NHS has faced rising demand for healthcare from a society in distress”.
– There has been a “surge” in multiple long-term conditions, including a rise in poor mental health among children and young people. Fewer children get their vaccines and fewer adults now participate in things such as breast cancer screening.
– Waiting times targets are being missed across the board, including for surgery, cancer care, A&E and mental health services. The report says “long waits have become normalised” and “A&E is in an awful state”, with long waits likely to be causing an additional 14,000 more deaths a year, according to the Royal College of Emergency Medicine. By April 2024, about one million people were waiting for mental health services. The overall NHS waiting list stands at 7.6 million.
– People are struggling to see their GP. “GPs are seeing more patients than ever before, but with the number of fully qualified GPs relative to the population falling, waiting times are rising and patient satisfaction is at its lowest ever level.”
– Cancer care still lags behind other countries and cancer death rates are higher than in other countries. There was “no progress whatsoever” in diagnosing cancer at stage I and II between 2013 and 2021. However, more recent figures show some improvement.
– Progress in cutting death rates from heart disease has stalled while rapid access to treatment has deteriorated. For example, the time for the highest-risk heart attack patients to have a rapid intervention to unblock an artery has risen by 28% from an average of 114 minutes in 2013-14 to 146 minutes in 2022-23.
– The NHS budget “is not being spent where it should be” and too great a share is being “spent in hospitals, too little in the community, and productivity is too low”. Too many hospital beds are taken up with people needing social care.
– Between 2009 and 2023 the number of nurses working in the community fell by 5%, while the number of health visitors dropped by nearly 20%.
– At the start of 2024, 2.8 million people were economically inactive due to long-term sickness, with most of the rise since the pandemic down to mental health conditions. The report said “being in work is good for wellbeing” and having more people in work grows the economy. “There is therefore a virtuous circle if the NHS can help more people back into work.”
– Raids on capital budgets have left the NHS with crumbling buildings and too many outdated scanners, and “parts of the NHS are yet to enter the digital era”. The report says the “NHS is in the foothills of digital transformation”.
– The NHS delayed, cancelled or postponed far more routine care during the pandemic than any comparable health system.
– Too many NHS staff are “disengaged” and there are “distressingly high-levels of sickness absence”. The pandemic was “exhausting” for many and the result has been a “marked reduction in discretionary effort across all staff groups”.
– Regulatory-type organisations now employ some 7,000 staff, or 35 per NHS provider trust, having doubled in size over the past 20 years.
On Hull Royal Infirmary’s maternity ward, inspectors noted that “systems, processes, and risk in the antenatal day unit / triage department were not well managed which led to long delays in women being seen and a chaotic environment which was not fit for purpose”.
They also flagged that “staff did not always work well together across the different units and some staff spoke about unkindness between staff”.
Writing about Blackpool Victoria Hospital’s urgent and emergency services unit, CQC inspectors observed that “at times, the department felt chaotic and we had concerns about the lack of oversight the leadership team had of the risks”.
Best performing hospitals
The CQC rated a total of 22 hospitals across the UK as ‘Outstanding’.
- Royal Surrey County Hospital
- East Surrey Hospital
- Homerton University Hospital
- Frimley Park Hospital
- Hexham General Hospital
- Queen Charlottes and Chelsea Hospital
- Chelsea and Westminster Hospital
- King’s Mill Hospital
- Conquest Hospital
- Fairfield General Hospital
- Moorfields Eye Hospital
- The Royal Marsden – London
- The Royal Marsden – Sutton
- Royal Papworth Hospital NHS Foundation Trust
- The Walton Centre
- Liverpool Heart and Chest Hospital
- Dental Hospital Manchester
- Royal Manchester Eye Hospital
- Leeds Dental Institute
- Thomas Linacre Centre
- Dental Hospital
- Wansbeck General Hospital
NHS review is shocking – but not surprising
By Sam Blanchard, Health Correspondent
LORD Darzi’s review is shocking but not surprising. It is grim to read all the NHS’s faults and failings in one place but people working in and around the health service knew what it would say long before it was written.
Unions and member organisations have been screaming about ‘challenges’ and ‘pressures’ for years, while millions of patients felt the same problems as anger and agony.
We already knew patients were waiting too long, dying too soon and crying out for help. So, too, are staff who worked their fingers to the bone through the pandemic thinking things would improve when Covid blew over – only to find better times never came.
Two of Lord Darzi’s three main explanations are ‘political choices’ (the Covid pandemic is number three), which gives Labour a free pass to blame the Tories – but Starmer and Streeting must turn bark into bite, and fast.
They say they cannot raise taxes for it and any extra cash would risk being taken from budgets needed for Britain’s many other crises, the Health Secretary admitted in a speech last night.
Darzi’s review calls for more money for GPs – but overloaded hospitals won’t open their purses. It calls for spending on new technology and modern buildings – but staff will strike again without pay rises.
There is no magic money tree and no magic medicine tree, either. Many of the problems are baked in for years to come: we can improve public health and urge Brits to live healthier lifestyles but that could take a generation to have an impact.
The diagnosis is as clear as it can be. Any prescription from Labour will anger somebody somewhere, but it must be unflinching and government and the NHS must actually commit to it for a decade or more
CQC inspectors thought the following 152 hospitals had room to improve their services:
- Luton and Dunstable Hospital
- Leicester General Hospital
- Leicester Royal Infirmary
- Gloucestershire Royal Hospital
- Kettering General Hospital
- Worcestershire Royal Hospital
- Royal Shrewsbury Hospital
- The Princess Royal Hospital
- Macclesfield District General Hospital
- Yeovil District Hospital
- Stepping Hill Hospital
- Musgrove Park Hospital
- Leighton Hospital
- Southport and Formby District General Hospital
- Ormskirk District General Hospital
- Bassetlaw District General Hospital
- Doncaster Royal Infirmary
- Montagu Hospital, Mexborough
- North Middlesex University Hospital
- Royal United Hospital Bath
- Stroud Maternity Hospital
- Royal Devon & Exeter Hospital (Wonford)
- North Devon District Hospital
- Great Western Hospital
- Horton General Hospital
- Pinderfields Hospital
- Dewsbury and District Hospital
- Queen Elizabeth Hospital Birmingham
- The Queen Elizabeth Hospital
- The County Hospital
- Norfolk and Norwich University Hospital
- Torbay Hospital
- Crowborough Birthing Centre
- Inspire Neurocare Worcester
- Maidstone Hospital
- The Tunbridge Wells Hospital at Pembury
- Princess Royal Hospital
- The Countess of Chester Hospital
- St Richard’s Hospital
- Worthing Hospital
- Royal Sussex County Hospital
- Freeman Hospital
- Royal Victoria Infirmary
- University Hospital Lewisham
- Queen Elizabeth Hospital
- King George Hospital
- Queen’s Hospital
- William Harvey Hospital
- Queen Elizabeth The Queen Mother Hospital
- Royal Derby Hospital
- Queens Hospital
- Chorley and South Ribble Hospital
- Royal Preston Hospital
- Russells Hall Hospital
- University Hospital Aintree
- New Royal Liverpool University
- Cumberland Infirmary
- West Cumberland Hospital
- George Eliot NHS Hospital
- Cheltenham General Hospital
- Lister Hospital
- Dorset County Hospital
- Basildon University Hospital
- Broomfield Hospital
- Southend University Hospital
- Manor Hospital
- Poole Hospital
- Queen’s Medical Centre
- University College Hospital & Elizabeth Garrett Anderson Wing
- Royal Lancaster Infirmary
- Furness General Hospital
- St George’s Hospital (Tooting)
- St James’s University Hospital
- Arrowe Park Hospital
- Lincoln County Hospital
- Saint Mary’s Hospital
- Wythenshawe Hospital
- North Manchester General Hospital
- Chesterfield Royal Hospital
- Southampton General Hospital
- St Mary’s Hospital
- Scarborough Hospital
- Royal Stoke University Hospital
- The Princess Alexandra Hospital
- Peterborough City Hospital
- Hinchingbrooke Hospital
- James Paget Hospital
- Airedale General Hospital
- The Royal Free Hospital
- Colchester General Hospital
- Medway Maritime Hospital
- John Radcliffe Hospital
- Alexandra Hospital
- St Peter’s Hospital
- Castle Hill Hospital
- Derriford Hospital
- Royal Cornwall Hospital
- St Austell Hospital – Penrice Birthing Unit
- Northampton General Hospital
- King’s College Hospital
- Croydon University Hospital
- South Tyneside District Hospital
- Sunderland Royal Hospital
- Princess Royal University Hospital
- County Hospital
- Salford Royal Hospital
- Royal Oldham Hospital
- Royal Hallamshire Hospital
- Northern General Hospital
- Jessop Wing
- Diana Princess of Wales Hospital
- Scunthorpe General Hospital
- Glenfield Hospital
- Pontefract Hospital
- Barking Birth Centre
- Whipps Cross University Hospital
- The Royal London Hospital
- University Hospital of Hartlepool
- University Hospital of North Tees
- Orpington Hospital
- Rotherham General Hospital
- Northwick Park Hospital
- Ealing Hospital
- Pilgrim Hospital
- Ashford Hospital
- Watford General Hospital
- Newham University Hospital
- Barnet General Hospital
- Westmorland General Hospital
- Kent & Canterbury Hospital
- West Suffolk Hospital
- The Ipswich Hospital
- St Albans City Hospital
- Hemel Hempstead General Hospital
- Victoria Infirmary
- Clatterbridge Hospital
- Mount Vernon Cancer Centre
- Queen Elizabeth II Hospital
- Queen Mary’s Hospital
- Central Middlesex Hospital
- Fleetwood Hospital
- Evesham Community Hospital
- Charing Cross Hospital
- Hammersmith Hospitals
- Sandwell General Hospital
- Manchester Royal Infirmary
- Weston Park Hospital
- Hannah House
- Ludlow Community Hospital
- Mount Gould Hospital
- Royal South Hants Hospital
- Mount Vernon Hospital
In response to Lord Darzi’s bombshell report – which found that A&E queues have exploded in size while progress in diagnosing cancer cases has stagnated – PM Keir Starmer declared the NHS “broken”.
He insisted the NHS must “reform or die”, setting out a 10-year plan to do so.
Keir’s 10-year plan for the NHS
THE Prime Minister said the Government is working on a 10-year plan to transform the NHS. This includes:
- Digital Transformation: transition to digital healthcare with innovations like fully digital patient records and the NHS app for self-referrals and data transparency.
- Community-Based Care: shift care from hospitals to local communities, increase GP access, and offer virtual consultations and home-based care through virtual wards.
- Prevention Focus: prioritise prevention with NHS health checks, early interventions, and focus on children’s mental health and dental care.
- Integrate Health and Social Care: streamline health and social care to reduce hospital stays and free up resources.
- Workforce Support: end NHS strikes and employ trainee GPs to strengthen the healthcare workforce.
- Long-Term Commitment: a decade-long reform plan to future-proof the NHS